Hypertensive disorders in pregnancy are some of the leading causes of maternal and fetal morbidity and mortality globally. These disorders, which include gestational hypertension, preeclampsia, and eclampsia, are estimated to complicate 5-10% of pregnancies. At Sitaram Bhartia hospital Delhi, a dedicated team works round-the-clock to provide comprehensive care to mothers with hypertensive disorders. Timely diagnosis and appropriate management are key to preventing adverse outcomes in such high-risk pregnancies.
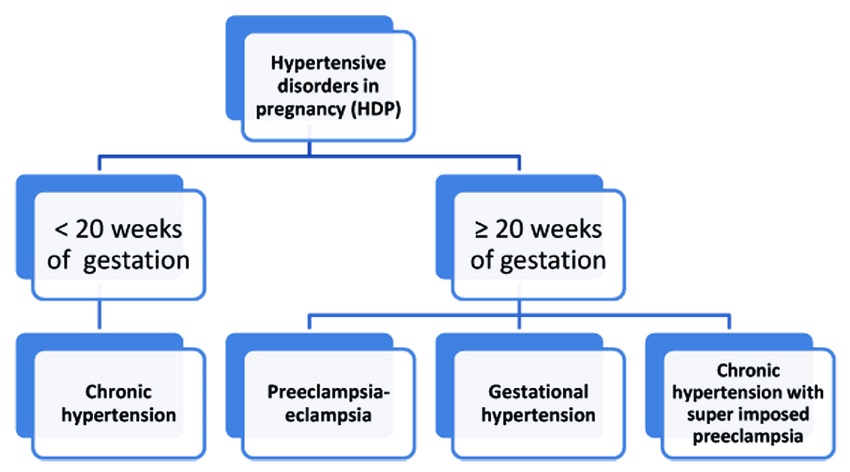
Hypertension in pregnancy refers to high blood pressure arising de novo after the 20th week of gestation. It usually occurs in women who had normal blood pressure prior to conception. Gestational hypertension is defined as systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg. If it coincides with proteinuria ≥300 mg/day, the condition is termed preeclampsia. Some women may present with preeclampsia even earlier in pregnancy, underscoring the need for close monitoring. When left unchecked, preeclampsia can progress to eclampsia which is characterized by seizures, visual disturbances, severe hypertension, hematological and liver function abnormalities.
The definitive treatment of hypertensive disorders in pregnancy is delivery. However, the timing and mode of delivery depend on the severity, gestational age, and response to expectant management. The latter involves close surveillance - both inpatient and outpatient, fetal surveillance, BP control, and prevention of seizures and other complications under the care of the best gynaecologist in delhi. Antihypertensive drugs like labetalol, nifedipine, and methyldopa are considered safe in pregnancy. Magnesium sulfate is the agent of choice for seizure prophylaxis in severe preeclampsia and eclampsia.
Some risk factors which predispose women to hypertensive disorders of pregnancy include:
- Primigravida status
- Maternal age ≥40 years
- Obesity
- Family history of preeclampsia
- Multiple pregnancy
- Preexisting hypertension/kidney disease/diabetes
The exact pathogenesis remains unclear but is likely multifactorial. Abnormal placentation early in pregnancy triggers an exaggerated maternal inflammatory response and systemic endothelial dysfunction. This results in vasoconstriction, hypertension, and end-organ ischemia. Both maternal and fetal genetic factors also play a role.
Adverse effects on the mother can be acute or long-term. Acute complications encompass hemorrhagic stroke, liver hematoma/rupture, acute kidney injury, pulmonary edema, and disseminated intravascular coagulation. Chronic hypertension, ischemic heart disease, and CKD occur more frequently in later life after having preeclampsia.
For the fetus and newborn, risks include placental abruption, intrauterine growth restriction (IUGR), preterm birth and perinatal mortality. Being born small for gestational age predisposes them to adulthood obesity, diabetes and hypertension via developmental programming. Newborns may also suffer complications of prematurity and severe illness at birth.
Given the heavy burden of hypertensive disorders in pregnancy, further research to elucidate genetic markers, refine screening tests, discover targets for drug therapy and prevent chronic diseases is the need of the hour. Global health initiatives promoting antenatal care utilization, task sharing for blood pressure monitoring and access to emergency obstetric services are other major priorities. Comprehensive care clinics such Sitaram Bhartia hospital Delhi serve as excellent platforms for managing high-risk pregnancies while advancing research on this important cause of maternal mortality worldwide.

No comments yet