Introduction:
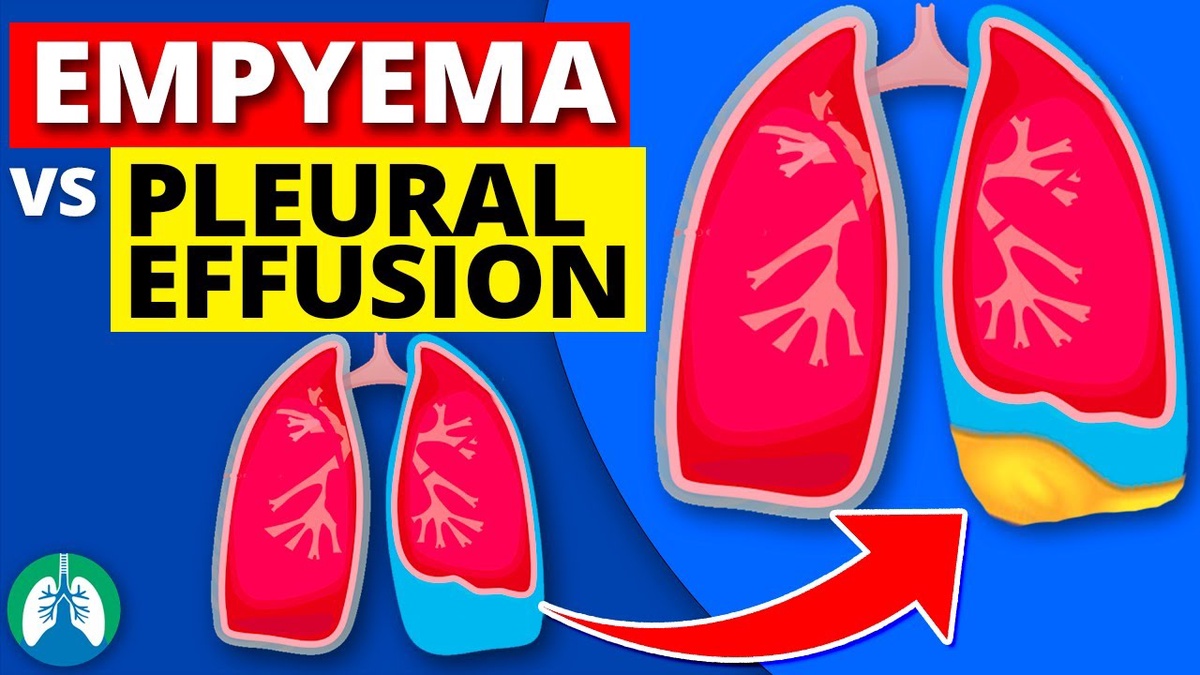
When it comes to respiratory issues, distinguishing between conditions is crucial for accurate diagnosis and effective treatment. Two commonly confused conditions are empyema and pleural effusion. While both involve the accumulation of fluid in the pleural space surrounding the lungs, they have distinct characteristics, causes, and treatment approaches. In this blog post, we will delve into the nuances of empyema and pleural effusion, helping you understand how to differentiate between the two.
Explore the nuanced differences between Empyema vs Pleural Effusion: Differentiating between the two conditions with the expertise of renowned pulmonologist, Dr. Harsh Vardhan Puri. This informative guide delves into the distinctive characteristics, diagnostic approaches, and treatment modalities for these two thoracic conditions. Gain a deeper understanding of the complexities involved in distinguishing between Empyema and Pleural Effusion, as Dr. Harsh Vardhan Puri sheds light on key aspects to aid both healthcare professionals and patients in navigating these respiratory challenges. Trust the expertise of Dr. Harsh Vardhan Puri for a comprehensive exploration of these pulmonary disorders, empowering you with knowledge for better health outcomes.
Understanding Pleural Effusion:
Pleural effusion refers to the abnormal accumulation of fluid in the pleural cavity, the space between the layers of the pleura – a thin membrane that surrounds the lungs and lines the chest cavity. This fluid buildup can result from various underlying causes, including congestive heart failure, pneumonia, liver disease, and malignancies.
Key Features of Pleural Effusion:
-
Fluid Composition:
- The fluid in pleural effusion is typically a transudate or exudate.
- Transudative effusions are often associated with systemic conditions like heart failure.
- Exudative effusions are usually a result of inflammation, infection, or malignancy.
-
Inflammation:
- Pleural effusion is generally non-inflammatory, with minimal or no infection.
- Inflammatory markers may be present, but infection is not a primary characteristic.
-
Common Causes:
- Heart failure, pneumonia, liver cirrhosis, and malignancies are common causes of pleural effusion.
- It can also occur as a complication of pulmonary embolism or autoimmune diseases.
Understanding Empyema:
Empyema, on the other hand, is a more specific condition characterized by the presence of pus in the pleural cavity. It is often a complication of bacterial pneumonia, lung abscess, or chest trauma. Unlike pleural effusion, empyema indicates an infectious process involving the pleura.
Key Features of Empyema:
-
Fluid Composition:
- The fluid in empyema is purulent, containing a significant amount of white blood cells, bacteria, and debris.
- The presence of pus distinguishes empyema from other forms of pleural effusion.
-
Inflammation:
- Empyema is inherently an inflammatory process, involving an infection within the pleural space.
- The infection triggers a more robust immune response, leading to the formation of pus.
-
Common Causes:
- Bacterial pneumonia, lung abscess, and chest trauma are common causes of empyema.
- It can result from the spread of infection from the lungs to the pleura.
Differentiating Factors:
-
Fluid Analysis:
- Analyzing the fluid obtained through thoracentesis is crucial.
- Presence of pus, high white blood cell count, and positive bacterial cultures suggest empyema.
-
Underlying Conditions:
- Understanding the patient's medical history and identifying associated conditions can aid in differentiation.
- Pleural effusion is often secondary to systemic issues, while empyema is more localized and infection-driven.
-
Clinical Presentation:
- Symptoms of empyema may include fever, chest pain, and purulent sputum, indicating an infectious process.
- Pleural effusion symptoms are more diverse, reflecting the underlying cause.
Conclusion:
In summary, while both empyema and pleural effusion involve the accumulation of fluid around the lungs, they differ significantly in terms of composition, inflammation, and underlying causes. Proper diagnosis requires a thorough understanding of the patient's medical history, clinical presentation, and fluid analysis. Timely and accurate differentiation is crucial for initiating appropriate treatment strategies and improving patient outcomes.

No comments yet