Diabetes, a chronic condition characterized by high blood sugar levels, affects millions worldwide. Among its many complications, one of the most concerning is the development of foot infections and ulcers in diabetic individuals. These conditions pose significant health risks and contribute to a considerable burden on healthcare systems globally. Understanding the intricacies of diabetic foot infections, diabetic sores, leg ulcers, and diabetic leg ulcers is crucial for effective prevention and management.
Diabetic Foot Infections: The Silent Threat
Diabetic foot infection is a common and potentially severe complication of diabetes. They typically arise from minor cuts, scrapes, or injuries to the foot that goes unnoticed due to diabetic neuropathy—a condition causing decreased sensation in the extremities. Because of this diminished sensation, individuals with diabetes may not realize they have sustained an injury, allowing infections to develop unchecked.
Diabetic Sores and Leg Ulcers: A Consequence of Poor Wound Healing
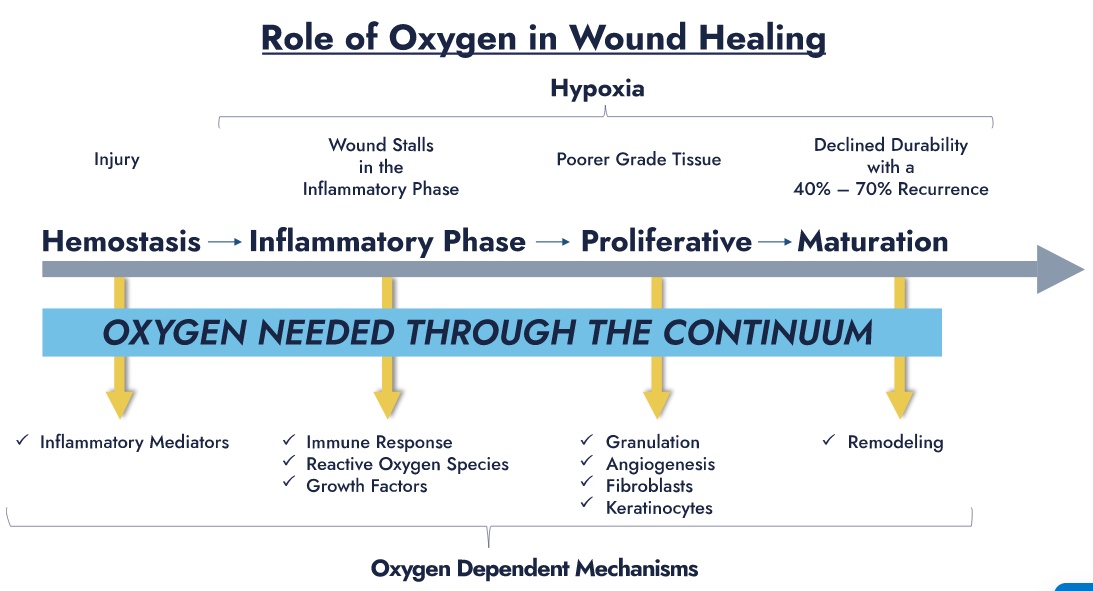
Furthermore, diabetic sores often impair the body's ability to heal wounds efficiently. High blood sugar levels can damage blood vessels and reduce circulation, depriving the affected area of essential nutrients and immune cells for fighting infections. As a result, even minor wounds can quickly progress into severe infections, leading to tissue damage, ulceration, and, in severe cases, limb amputation.
Diabetic foot ulcers, also known as diabetic sores, are open wounds or sores commonly occurring on the feet of individuals with diabetes. These ulcers develop when minor injuries or pressure points on the foot fail to heal properly, often due to poor circulation and nerve damage associated with diabetes. These ulcers can become infected without timely intervention, leading to further complications.
Leg ulcers, another prevalent issue in diabetic individuals, can occur due to a variety of factors, including poor circulation, peripheral artery disease, and venous insufficiency. Diabetes exacerbates these underlying conditions, making individuals more susceptible to developing leg ulcers. Like diabetic foot ulcers, leg ulcers in diabetic patients are prone to infection and slow healing, increasing the risk of complications and necessitating comprehensive wound care management.
Challenges in Management and Prevention
Managing diabetic leg ulcers present numerous challenges for patients and healthcare providers. The complex interplay of factors contributing to these conditions requires a multidisciplinary approach encompassing wound care specialists, podiatrists, endocrinologists, and other healthcare professionals.
Prevention remains the cornerstone of diabetic foot care. Individuals with diabetes must practice meticulous foot hygiene, inspect their feet regularly for any signs of injury or infection, and wear appropriate footwear to minimize the risk of foot trauma.
Managing diabetic leg ulcers present numerous challenges for patients and healthcare providers.
Early detection and prompt treatment of foot infections and ulcers are paramount in preventing complications. Any signs of infection, such as redness, warmth, swelling, or drainage from a wound, should prompt immediate medical attention. Healthcare providers may prescribe antibiotics to treat diseases and implement wound care strategies such as debridement, offloading pressure from the affected area, and applying specialized dressings to promote healing.
In cases where ulcers become severe or fail to respond to conservative treatments, surgical intervention may be necessary to remove infected tissue or restore blood flow to the affected area. However, preventing the progression of ulcers to this stage through diligent foot care and proactive management remains the preferred approach.
Conclusion
Diabetic foot infections and ulcers represent a significant healthcare challenge with potentially devastating consequences for affected individuals. The combination of impaired wound healing, neuropathy, and vascular complications characteristic of diabetes underscores the importance of proactive prevention and comprehensive management strategies.
By promoting awareness, early detection, and timely intervention, healthcare providers can help mitigate the impact of diabetic foot infections and ulcers, ultimately improving outcomes and quality of life for individuals with diabetes. Through collaborative efforts between patients, caregivers, and healthcare professionals, we can strive towards reducing the prevalence and severity of these complications, alleviating the burden they impose on individuals and healthcare systems.
For more information about diabetic leg ulcers, tap to Advanced Oxygen Therapy Inc. for the best treatment for diabetic disease or ulcers.

No comments yet