Diabetes, a chronic condition affecting millions worldwide, can lead to a myriad of complications, including diabetic leg ulcers and foot infections. These conditions pose significant health risks and severely impact an individual's quality of life. Understanding the causes, symptoms, and treatment options for diabetic leg ulcers and foot infections is crucial for effective management and prevention.
What are Diabetic Leg Ulcers and Foot Infections?
Diabetic leg ulcers and foot infections are complications commonly associated with diabetes mellitus. Leg ulcers are open wounds or sores that typically occur on the lower legs or feet. In diabetic individuals, these ulcers often develop due to poor circulation, nerve damage (neuropathy), and impaired wound healing.
Diabetic foot infections, on the other hand, occur when bacteria enter through breaks in the skin, such as cuts, sores, or ulcers, leading to localized infection. If left untreated, these infections can quickly escalate, spreading to deeper tissues and even bones.
Causes and Risk Factors
Several factors contribute to the development of diabetic leg ulcers and foot infections:
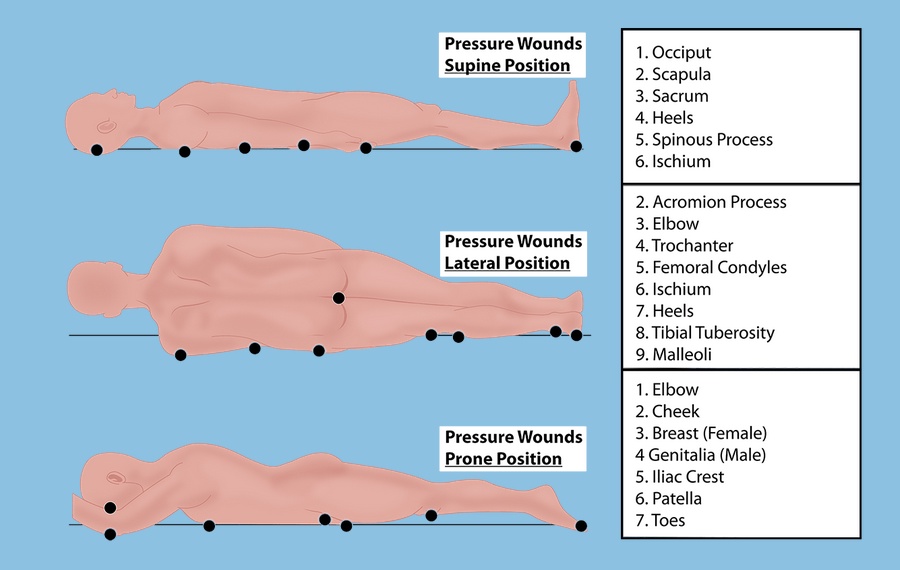
Peripheral Neuropathy: Diabetic sores can damage nerves, particularly those in the feet and legs, leading to loss of sensation. Individuals may not feel minor injuries or pressure, allowing untreated wounds to go unnoticed.
Poor Circulation: Diabetes can impair blood flow to the lower extremities, reducing the delivery of oxygen and nutrients necessary for wound healing. Reduced circulation also increases the risk of infection and delays healing.
Foot Deformities: Conditions like hammertoes, bunions, and Charcot foot (a condition causing weakening of the bones in the foot) can increase pressure and friction, leading to the formation of ulcers.
Uncontrolled Blood Sugar Levels: High blood sugar levels can impair the immune system's ability to fight infections and hinder the body's natural healing processes.
Smoking: Smoking further impairs circulation and reduces the body's ability to heal wounds, significantly increasing the risk of complications in diabetic individuals.
Symptoms
Recognizing the signs and symptoms of diabetic leg ulcers and foot infections is essential for prompt intervention:
Leg Ulcers may appear as open sores or wounds, typically on the lower legs or feet. The surrounding skin may be discolored, swollen, and warm. In some cases, drainage or pus may be present.
Foot Infections: Symptoms of foot infections include redness, warmth, swelling, pain, and drainage from the affected area. Fever and chills may also indicate a systemic infection requiring immediate medical attention.
Treatment and Management
Early detection and proper management are crucial for preventing complications associated with diabetic leg ulcers and foot infections:
Wound Care: Proper wound care promotes healing and prevents infection. This may include cleaning the wound with mild soap and water, applying antibiotic ointments, and covering it with sterile dressings.
Offloading Pressure: Offloading pressure from the affected foot or leg helps relieve stress on the wound, promoting healing. This may involve wearing particular footwear, using orthotic devices, or avoiding activities that exacerbate pressure on the affected area.
Antibiotic Therapy: In cases of foot infections, antibiotics are prescribed to combat bacterial growth and prevent the spread of disease. The antibiotic choice depends on the infection's severity and the type of bacteria involved.
Wound Debridement: In some cases, non-healing ulcers may require surgical debridement, where dead or infected tissue is removed to facilitate healing.
Managing Blood Sugar Levels: Tightly controlling blood sugar levels through diet, exercise, and medication prevents complications and promotes wound healing.
Vascular Interventions: In individuals with significant peripheral artery disease, vascular interventions such as angioplasty or bypass surgery may be necessary to improve blood flow to the affected limbs.
Prevention of diabetic foot infection
Preventing diabetic foot infection is critical to reducing the risk of complications:
Foot Care: Daily inspection of the feet for cuts, sores, or blisters is essential. Keeping the feet clean, moisturized, and dry helps prevent skin breakdown.
Proper Footwear: Wearing well-fitted shoes that provide adequate support and cushioning helps prevent pressure points and reduce the risk of foot injuries.
Regular Foot Exams: Regular foot exams by a healthcare professional, especially for individuals with diabetes, can help identify potential problems early and prevent complications.
Blood Sugar Control: Maintaining tight control of blood sugar levels through diet, exercise, and medication helps prevent nerve damage and promotes wound healing.
In conclusion, diabetic leg ulcers and foot infections are serious complications that require prompt intervention and comprehensive management. By understanding the causes, symptoms, and treatment options, individuals with diabetes can take proactive steps to prevent these complications and maintain optimal foot health. Regular monitoring and adherence to preventive measures are essential for minimizing the risk of complications and preserving overall well-being.
For more information about diabetic foot infection, switch to Advanced Oxygen Therapy Inc. for the best wound care or healing programs.

No comments yet