What Happens If Too Much Carbon Dioxide Builds Up in Your Blood?
If too much carbon dioxide builds up in your blood, it can cause a number of problems. Some of these are more serious than others.
If you’re experiencing fatigue, weakness, or other symptoms, your provider may order a CO2 blood test. This quick blood draw checks your body’s balance of electrolytes and tells your health care provider what your symptoms mean.
High Carbon Dioxide Levels
What happens if too much carbon dioxide builds up in your blood?
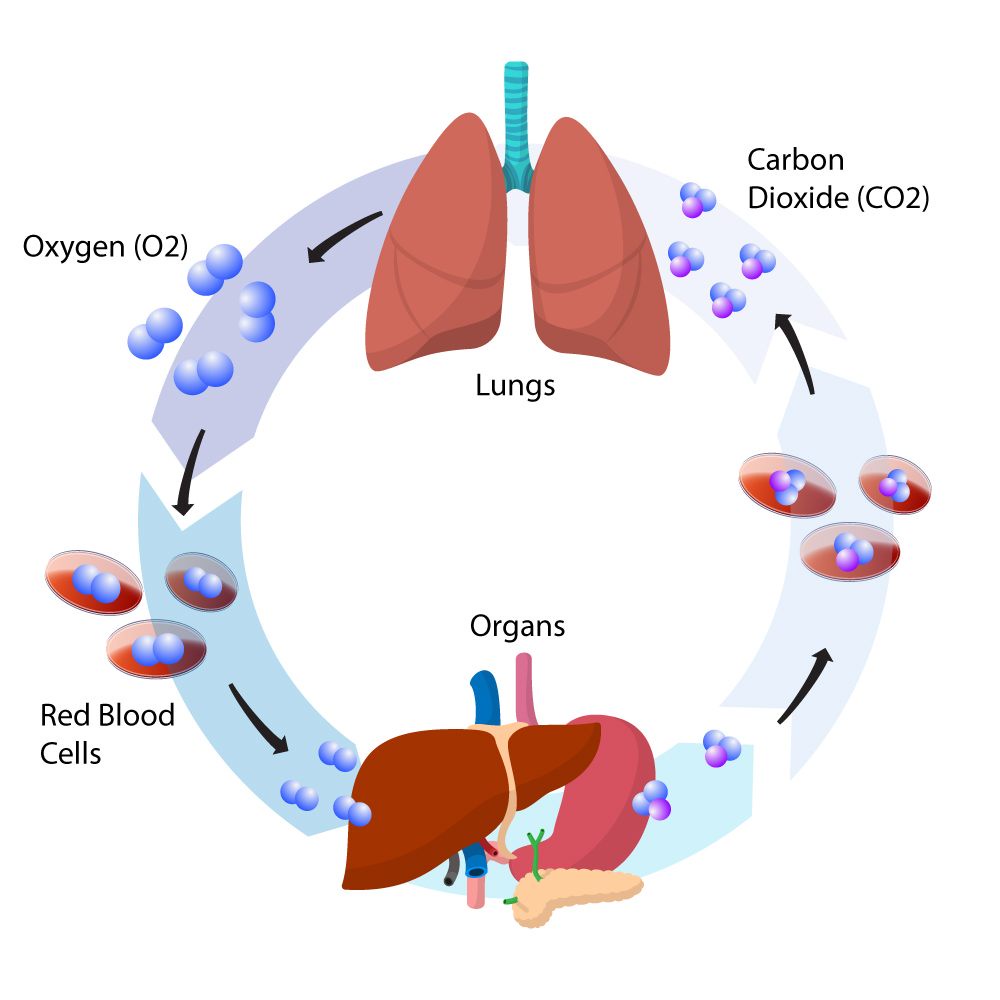
Carbon dioxide is a waste product your body produces as part of the natural processes of breathing. Your lungs take in the CO2 from your blood, and then exhale it out of your body. This process happens all day, every day.
Most of the CO2 in your body is dissolved in the form of bicarbonate (HCO3-), which helps regulate your pH balance. When your blood's pH becomes too acidic or basic, the bicarbonate will become dissolved.
However, if you lose too much CO2 in your body, it may cause problems with your lungs with Nitrous Oxide. Your lungs can't keep up with the demand for oxygen, and this can lead to respiratory disorders such as hypercapnia or respiratory acidosis.
A CO2 blood test can detect these symptoms and help your doctor determine whether they are a serious problem or not. The test is usually part of an electrolyte panel, a basic metabolic panel or a comprehensive metabolic panel that's part of your health checkup.
This test uses a small needle to get a sample of your blood from a vein in your arm. The sample of blood will be diluted with an acid to unlock the bicarbonate and measure the amount of carbon dioxide in your blood.
The bicarbonate in your blood is a type of electrolyte, which helps maintain the balance of acids and bases in your body (pH balance). An imbalance of electrolytes can be caused by an electrolyte deficiency, a kidney disease, or a lung disease.
Your healthcare provider will order the test when you have a routine physical exam or if there is a possibility that you are developing an electrolyte imbalance. Your CO2 blood test is usually ordered as a part of an electrolyte panel, but can also be used as a stand-alone test.
Your CO2 blood test is a non-invasive, painless procedure that can be done in a lab. Your healthcare provider will tell you if you need to fast (not eat or drink) for several hours before the test. You may also need to stop taking certain medicines before the test.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a lung disease that is often caused by smoking, but some people who have never smoked can get it as well. If you have this disease, it will affect the way you breathe and may make it difficult to do the things you want to do.
The lungs are very important to your health, and they play a vital role in taking oxygen into your body and throwing out carbon dioxide when you exhale. Your lungs do this all day, every day.
Usually, your lungs use the natural elasticity of the small airways in your lungs to force air out of your body when you breath in and out. However, with COPD, your lungs lose their elasticity, and they can’t force enough air out. This causes too much carbon dioxide to build up in your lungs and your blood.
Your doctor will do a physical exam to check your breathing and check for any signs of COPD. He or she will also listen to your lungs with a stethoscope. If you have wheezing, a long expiratory (breathing) time or you have trouble catching your breath, these are all signs of COPD and Hydrogen gas.
If you are diagnosed with COPD, your doctor will talk to you about your symptoms and what the treatment plan is going to be. Depending on your specific condition, you may need to take medications and use breathing machines.
Another possible treatment is oxygen therapy. You may need it all the time or only at certain times. Oxygen helps you breathe better, so you can do the things you want to do and stay healthy.
Your doctor might suggest medicines called bronchodilators, which relax your bronchial muscles. Using these medicines can reduce the severity of your symptoms and make them easier to manage.
In addition, you might need medication to help control your cough. Coughing can cause mucus to build up in your lungs, and this can irritate your breathing. Your doctor might also prescribe antibiotics or steroids to help with your symptoms.
If you have COPD, your doctor might recommend a program of exercise to help keep your lungs healthy and improve your quality of life. Walking can be very helpful, but it’s important to slowly increase the distance you walk and not talk when you are doing this activity.

image source https://www.pinterest.ph/
Hypercapnia
If you have a condition that limits your breathing, like COPD or asthma, you can develop too much carbon dioxide in your blood. This condition is called hypercapnia, and it may be a sign of a more serious problem.
When there's too much carbon dioxide in your blood, it can make you feel weak, tired and short of breath. It can also cause problems with your heart and lungs. It can make your skin and eyes sting or itchy, or it can cause confusion and agitation.
Your doctor will use a combination of tests to find out what's causing the high carbon dioxide levels and to determine the best treatment for you. They will also consider your symptoms, if any, and any other risk factors for developing hypercapnia.
Some health conditions can cause hypercapnia, such as chronic obstructive pulmonary disease (COPD), sleep apnea and exercise-induced hyperventilation. Symptoms of these conditions can range from mild to severe, and they're important to watch for if they happen frequently or are worsening over time.
In other cases, hypercapnia is caused by a nerve or muscle disorder that prevents you from breathing properly. These disorders can include Guillain-Barre syndrome and muscular dystrophies.
Other disorders, such as brain tumors, can also cause hypercapnia by affecting your ability to breathe and exhale properly. Your physician can prescribe medication to help you get more oxygen into your lungs. They can also recommend breathing exercises and supplemental oxygen.
People who are at a higher risk of developing hypercapnia of Helium gas can also have genetic conditions that don't produce enough alpha-1-antitrypsin, a protein that helps your body's lungs work. This is common in people who have a history of lung or airway diseases, such as COPD and asthma.
Using supplemental oxygen can lower your blood carbon dioxide level and reduce the symptoms of hypercapnia. You'll breathe it in through a mask or nosepiece attached to tubes that connect it to a device that filters and provides a steady stream of oxygen. It can also be used during surgery and other medical procedures.

image source https://www.pinterest.ph/
Respiratory Acidosis
Normally, the body's respiratory system balances the ions that make your blood and other bodily fluids acidic. When the body doesn't have the ability to do this, it can cause acidosis, which lowers your blood pH below safe levels.
When this happens, you need medical attention. If it is severe enough, you can suffer organ failure and even death.
It's important to know what the symptoms of respiratory acidosis are so that you can get treatment as quickly as possible. These include fatigue, confusion, and drowsiness.
A doctor can diagnose respiratory acidosis by doing a physical exam, blood tests for carbon dioxide and acid levels, and lung function testing. They may also use X-rays or other imaging tests to look at your lungs and help find the cause of your acidosis with ethylene oxide gas.
Most cases of respiratory acidosis happen when your lungs can't get rid of enough CO2 during breathing, or you have an underlying disease that causes your lungs to not function properly. These can include asthma, chronic obstructive pulmonary disease (COPD), emphysema, and pneumonia.
Your doctor can check the amount of carbon dioxide that's expelled from your lungs with a gas diffusion test or an exercise test, both of which involve breathing in and out of a machine. This shows how your lungs work when you're breathing in and out of a machine, which can help them identify the causes of your acidosis.
Another way that your doctor can tell if you have acidosis is to perform a lung function test, which involves using a mask and a machine to measure how well your lungs can blow in and out air. This test is especially helpful if you have other medical conditions like heart problems, diabetes, or cancer.
Finally, your doctor can do other testing that can tell them if you have an underlying condition that is causing the problem. They might do a muscle test to see if your muscles are working properly, or an X-ray to look at the shape of your chest.
Ultimately, the goal of treating acidosis is to reduce the amount of carbon dioxide that's in your lungs. This can be done by changing your lifestyle, taking care of the underlying condition that's causing it, or by using medications.

No comments yet