Wound healing is a complex and crucial process that our bodies naturally undergo when we suffer injuries. However, for individuals living with diabetes, this process can be significantly compromised. Diabetes, a chronic metabolic disorder characterized by high blood sugar levels, can lead to complications, including impaired wound healing. This article will explore the intricate relationship between diabetes and wound healing, focusing on pressure ulcer care, chronic wounds, and the unfortunate consequences of lower limb amputations.
Diabetes and Wound Healing
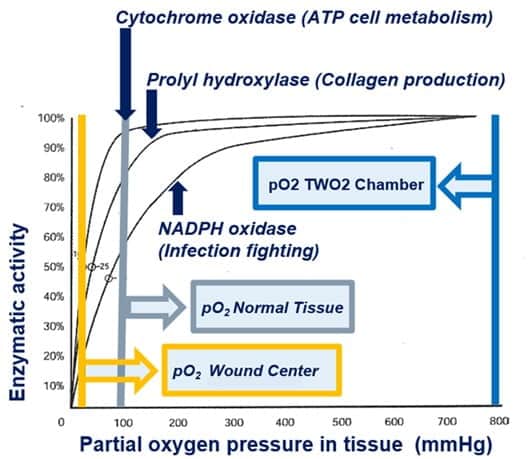
wound healing and diabetes are intrinsically connected. High blood sugar levels can damage blood vessels and nerves, reducing blood flow to the extremities, particularly the feet. This diminished circulation deprives tissues of essential oxygen and nutrients, slowing the body's ability to repair and regenerate damaged cells. Furthermore, diabetes can lead to neuropathy, a condition characterized by nerve damage, causing a loss of foot sensation. Consequently, individuals with diabetes may not realize they have a wound, making it more susceptible to infection and complications.
Pressure Ulcer Care, the best action to prevent ulcers
Pressure ulcers, also known as bedsores or pressure sores, are a common concern for individuals with diabetes, particularly those who are bedridden or have limited mobility. These ulcers typically develop over bony prominences such as the heels, sacrum, and hips due to prolonged pressure and friction. For diabetics, the risk of pressure ulcers is heightened due to the compromised blood flow and sensory perception.
pressure ulcer care in diabetic individuals involves a multifaceted approach:
Skin Inspection: Regularly inspect the skin, especially over bony areas, to identify early signs of redness or irritation. Early detection is critical to preventing pressure ulcers from worsening.
Positioning: Frequent repositioning is essential to relieve pressure on vulnerable areas. Bedridden individuals should be turned and repositioned every few hours, and those in wheelchairs should shift their weight regularly.
Support Surfaces: Specialized support surfaces, such as pressure-relieving mattresses and cushions, can help distribute pressure more evenly and reduce the risk of ulcers.
Chronic Wounds
Diabetic individuals are prone to developing chronic wounds, which are wounds that do not heal in the expected timeframe or exhibit delayed healing. These wounds can be particularly challenging to manage due to the underlying issues associated with diabetes. Chronic wound in people with diabetes include diabetic foot ulcers and venous leg ulcers.
Chronic wound in people with diabetes include diabetic foot ulcers and venous leg ulcers.
Effective management of chronic wounds in diabetes involves the following measures:
Wound Assessment: Thoroughly assess the wound, including its size, depth, and surrounding tissue condition. This evaluation guides the choice of appropriate treatment strategies.
Infection Control: Chronic wounds are more susceptible to infection. Administer antibiotics when necessary and monitor for signs of infection, such as redness, warmth, swelling, or pus.
Debridement: Remove dead or unhealthy tissue from the wound to promote healing. Debridement can be done through various methods, including surgical, enzymatic, or autolytic.
Lower Limb Amputation
One of the most devastating consequences of poorly managed diabetes and its impact on wound healing is lower limb amputation. When chronic wounds or diabetic foot ulcers become severely infected or fail to heal despite all efforts, amputation may be the last resort to prevent the spread of infection and save the patient's life.
The psychological and physical toll of lower limb amputation is profound, affecting a person's mobility, independence, and overall quality of life. To reduce the risk of amputation, diabetic individuals must take proactive steps in managing their condition:
Regular Foot Care: Inspect your feet daily for any signs of wounds, blisters, or changes in skin color. Promptly seek medical attention for any abnormalities.
Blood Sugar Control: Maintain optimal blood sugar levels through medication, diet, exercise, and regular monitoring.
Conclusion
Wound healing in diabetes is complex and challenging, requiring a comprehensive approach that includes diligent wound care, infection control, and proactive measures to prevent complications. Pressure ulcer care, management of chronic wounds, and the prevention of lower limb amputation are essential aspects of diabetes management. Individuals with diabetes must prioritize self-care, maintain optimal blood sugar levels, and seek timely medical intervention to address wound-related concerns. Additionally, healthcare professionals are crucial in educating patients about wound prevention and management strategies to enhance the overall well-being of those affected by diabetes. By addressing wound healing issues effectively, we can mitigate the devastating consequences of this condition and improve the quality of life for individuals with diabetes.

No comments yet